- Home
- About
- Partners
- Newcastle University
- University of L'Aquila
- University of Manchester
- Alacris Teranostics GmbH
- University of Pavia
- Polygene
- Consiglio Nazionale delle Ricerche
- INSERM
- Certus Technology
- Charité Universitaet Medizin
- GATC Biotech
- University Medical Center Hamburg Eppendorf
- Evercyte GmbH
- University Hospital of Cologne
- PRIMM Srl
- University of Freiburg
- University of Antwerp
- Finovatis
- Research
- SYBIL at a glance
- Bone
- Growth plate
- Desbuquois dysplasia
- Diastrophic dysplasia
- MCDS
- Osteopetrosis
- Osteoporosis
- Osteogenesis imperfecta
- Prolidase deficiency
- PSACH and MED
- Systems biology
- SOPs
- Alcian Blue staining
- Bone measurements
- BrdU labelling
- Cell counting using ImageJ
- Chondrocyte extraction
- Cre genotyping protocol
- DMMB assay for sulphated proteoglycans
- Densitometry using ImageJ
- Double immunofluorescence
- Electron microscopy of cartilage - sample prep
- Extracting DNA for genotyping
- Grip strength measurement
- Histomorphometry on unon-decalcified bone samples
- Immunocytochemistry
- Immunofluorescence
- Immunohistochemistry
- Quantitative X-ray imaging on bones using Faxitron and ImageJ
- Skeletal preps
- TUNEL assay (Dead End Fluorimetric Kit, Promega)
- Toluidine Blue staining
- Toluidine Blue staining
- Von Kossa Gieson staining
- Wax embedding of cartilage tissue
- Contact Us
- News & Events
- Links
- Portal
MCDS
Metaphyseal chondrodysplasia type Schmid (MCDS) is a dwarfism caused by mutations in a protein called type X (ten) collagen. MCDS is presents as child first starts to walk due to a waddling gait. X-rays show abnormalities with the ends of the bones and a hip dysplasia. Type X collagen is a protein made specifically by the hypertrophic (or large expanded) cells in the growth plate – the expansion of these cells are an important part of the bone growth process.
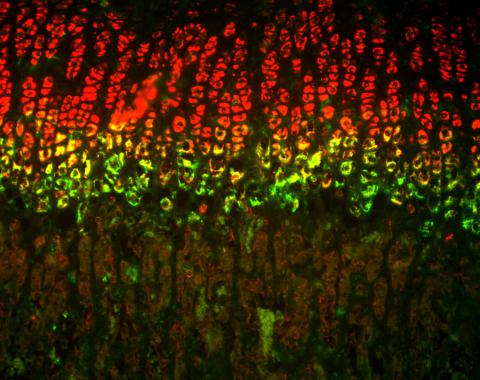
Double labelled in situ hybridisation showing cells expressing type II (two) collagen in red (the proliferating cells) and cells expressing the type X (ten) collagen in green (the hypertrophic cells). Image courtesy of Dr Helen Rajpar, University of Manchester
We know that many of the mutations in type X collagen produce a stress in hypertrophic chondrocytes that reduces the expansion of these cells causing reduced growth and resulting in dwarfism. The mutant type X collagen cannot be secreted by the hypertrophic chondrocytes and remains in the cells. Deposits of mutant type X collagen can be found inside the cells in the organelle called the endoplasmic reticulum (ER). This results in a important cell stress reaction called ER stress.
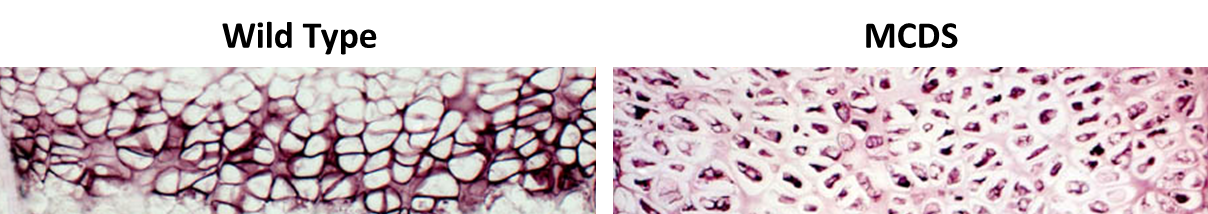
Immunohistchemistry staining (brown) for type X collagen in the hypertrophic zone of the growth plate. Image courtesy of Dr Louise Kung (University of Manchester)
However, there is one type of mutation causing MCDS that has not been studied in detail (premature stop codons) and these mutations may cause the reduced growth by a slightly different route. The researchers at the University of Manchester are developing a drug treatment that they believe will relieve the stress caused by the majority of mutant forms of type X collagen and may therefore be an effective therapy. Part of the programme of research is to test this treatment strategy in their model systems. The second aspect of the programme is to establish the mechanism by which premature stop codons in type X collagen induce the MCDS dwarfism and to test whether the stress-relieving treatments being developed are also effective in these cases.


